The Real Reason Weight-Loss Drugs Fail
and why your business model might collapse with it.
Right now, thousands of patients are beginning their GLP-1 journeys. They're imagining fitting into clothes they haven't touched in years, having newfound energy to play with their kids, and feeling hopeful about their health.
But for most, their GLP-1 journeys won't be smooth sailing. Instead, they’ll spend their nights doomscrolling Reddit searching for "how to stop nausea immediately," or "please god tell me these sulphur burps stop.
As a doctor in the GLP-1 space, I hear about these patients all the time. One even told me they were considering quitting GLP-1s because they couldn’t get through a single work meeting without ducking out to the bathroom to splash cold water on their face to ease the waves of nausea.
The early side effects of medications like Wegovy and Mounjaro can be pretty damn miserable: nausea, constipation, vomiting, and constant fatigue.
It’s enough discomfort to make patients question whether sticking it out is truly worth it.
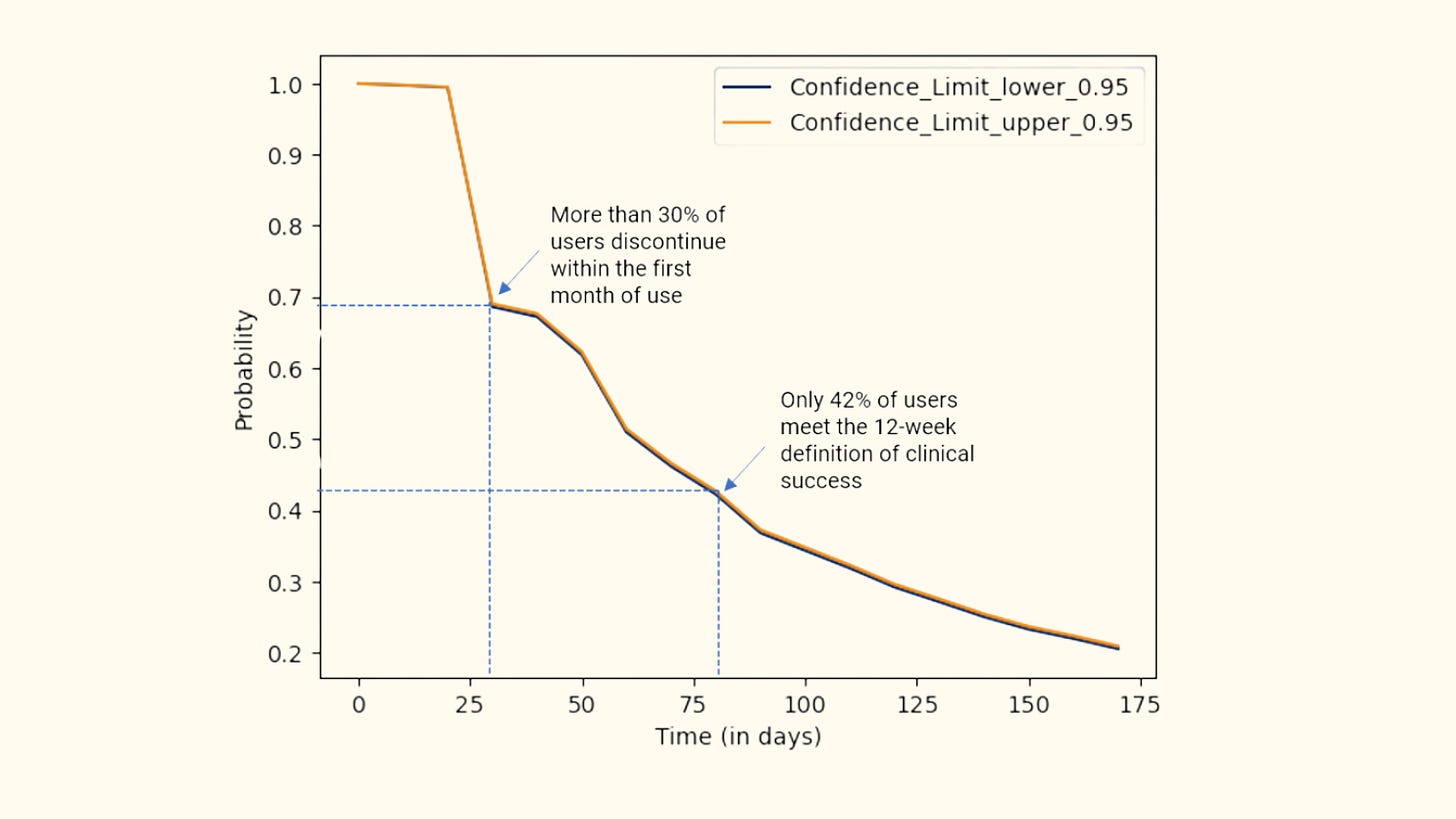
A recent Blue Cross Blue Shield analysis of over 169,000 GLP-1 patients found that 30% quit within the first four weeks, and nearly half dropped off before hitting 12 weeks.
For telehealth providers betting heavily on GLP-1s, the implications are devastating.
You’ve just said goodbye to future renewals, upsells, cross-sells and referrals. This is the difference between a $200 one-time transaction and a $5,000+ lifetime-value patient. More importantly, it's the difference between an unhappy customer who missed out on a transformative health outcome, and someone whose life has been positively changed forever.
The question becomes: Is there a way to address side effects before your patients churn—for good?
The Danger Zone
The Blue Cross analysis revealed that churn usually happens within the first six weeks of a patient's journey. I call this period the “danger zone”.
This is when patients face a double whammy. First, they get hit with the initial shock of side effects from the starter dose. Then, just as their bodies start adjusting, the second, increased dose triggers a fresh wave of side effects. It’s enough to push them over the edge—and straight out the door.
Your instinct might be, “Well, if we know exactly when patients churn, let’s ramp up CRM, SMS check-ins, app notifications, and provide extra support.”
The problem is most companies don’t do enough to predict who's going to suffer from side effects in the first place. Without this intel, you're forced to rely on a one-size-fits-all dosing schedule designed for labs, but patients don't live in labs. The real world is messy, and people are inconveniently human.
This traps you in a catch-22:
Escalate the doses to get results but side effects spike, causing churn.
Stick with the lowest dose to avoid side effects, and patients complain of not seeing results fast enough, causing churn anyway.
Neither path works.
Even if a patient sticks it out and survives the “danger zone,” the likelihood of them quitting at some point within the first year is truly abysmal.
A hotly debated JAMA analysis found that nearly two-thirds (64.8%) or 31,740 patients discontinued treatment, with most citing side effects as their primary reason for stopping.
Acquisition is easy. Retention is hard.
I don’t care how good your branding or marketing is. Once side effects become the reason patients quit, the negative association locks in and you've permanently lost around 1 in 5 patients—and they’ll never touch a GLP-1 again.
How do we prevent this? The solution is prediction, flexible and personalized dosing, and stepping in before your patients even realize they're considering quitting.
Stop Guessing, Start Predicting
You’re never going to nail prediction perfectly (at least, not yet). But you don’t need perfect—you just need useful. And useful is absolutely within reach.
Here's exactly what you can start doing right now:
1. Turn your churn into your strongest revenue driver
Your telehealth platform is already sitting on a goldmine of patient data. For the love of God, please, use it.
Start by building a simple predictive model to flag patients at high risk of developing side effects. Chinese researchers have already shown exactly how to do it. They developed a straightforward predictive "nomogram," that pinpoints which patients will struggle most. They zoned in on four factors that increase risk:
Being over 55
Female
Having existing gut issues like IBS and GERD
Taking multiple medications at once
Sure, most clinicians could’ve guessed these factors—but guessing isn’t actionable. More importantly, these are just the factors the Chinese researchers identified. Your data might reveal entirely different predictive signals unique to your patient population.
The key is to start building your own risk-stratification system now. From the very first consult, you should instantly flag high-risk patients—like a 60-year-old woman with IBS who's on multiple meds—and adjust her titration plan from day one.
Maybe she starts at a half-dose, or you space out her dose increases to prevent discomfort and keep her from churning.
Once you nail this, your upsells become genuinely contextual—not just random recommendations.
You’ll know exactly when nausea typically sets in and precisely when to offer supplements and fiber for constipation. Suddenly, your churn prevention strategy becomes precise and transforms retention into your strongest revenue driver. Kerching.
2. Get them Genes
The talk of the town is 23andMe filing for bankruptcy. Now, their genetic database which is 15 million people strong is up for grabs. Whoever snaps up this genetic treasure trove will know who's wired to struggle with GLP-1 therapy. They'll have data—presumably already mapped—to predict side effects, tolerability, and optimal dosing.
Now imagine this as your patient’s first consult:
"Your genetic data shows you carry a GLP-1R mutation. That means you'll probably need double the standard dose of Mounjaro, and unfortunately, you're predisposed to miserable nausea. But here's exactly how we'll manage that."
Any competitor can match your ads or your slick UX. But replicating a genetic database of 15 million people? Good luck. By snapping this up, you'd essentially control a data asset that no one can easily copy or quickly catch up to.
It’s the kind of competitive edge that investors dream about and competitors fear. It’s the one of the strongest moats imaginable.
Okay, so you'll need a spare $30-40 million. But if you're Hims, Ro—any of the big telehealth players—this acquisition is a no-brainer. It’s a direct path to market dominance.
If you're in the smaller leagues, your best play is blood testing your patients. While you won't get anywhere near the insights of genetic blueprinting, , you'll get biomarkers that might (might being the keyword) be helpful in predicting side effects and tolerability if you pair it up with a predictive risk stratification algorithm I mentioned above.
3. Attack of the Clones
I’m ABSOLUTELY convinced this is the future of GLP-1 therapy: a digital twin. It’s a virtual version of you, built from real-time data on your sleep, diet, stress, physical activity, and glucose levels. It’s like having a health avatar that knows exactly how you’re feeling (sometimes before you do).
One reason I’m so optimistic is a recent proof-of-concept trial by Twin Health. They ran a huge study with 1,850 type 2 diabetes patients. Each patient wore a continuous glucose monitor (CGM), Fitbit sensors, and smart scales, all integrated with a digital twin app that tracked their meals, sleep, exercise, stress, and medication use.
Twin’s algorithms then used all this data to adjust treatments on the fly, responding in real time to each patient's actual metabolic responses.
And the results were impressive:
89% hit optimal blood sugar (HbA1c below 7%)
Insulin use dropped 94%
Average weight loss was nearly 5 kg.
Adapting this to GLP-1 therapy isn't some crazy leap. You're already capturing most of the data you need—like sleep quality, activity levels, weight fluctuations, even stress—from your patients’ Apple Watches and Fitbits.
With some side effect data from your telehealth app, you just need to connect the dots in real time and observe how each patient's body responds after every GLP-1 dose.
With continuous, personalized data flowing in, predicting side effects becomes much more reliable. Once you can predict the side effects accurately, dose adjustments become pretty straightforward. You'll know when to prescribe off licence, space out doses, or hold steady for a week.
For you as a founder, the value is huge. Now you’ve got a highly personalized, proactive patient management that becomes scalable and automated.
Pens aren’t personal
The biggest barrier to true personalization in GLP-1 therapy is the delivery mechanism itself—the pens. It’s basically impossible to finely adjust doses when your entire treatment comes packaged in rigid increments.
So I was surprised when I came across a recent Diabetes Care paper describing a workaround called fractional dosing (please don’t call it microdosing, it reminds me of Bryan Johnson). Clinicians instruct patients to count audible "clicks" on standard GLP-1 pens to give smaller, fractional doses. Each pen has roughly 72 clicks, allowing for more precise adjustments.
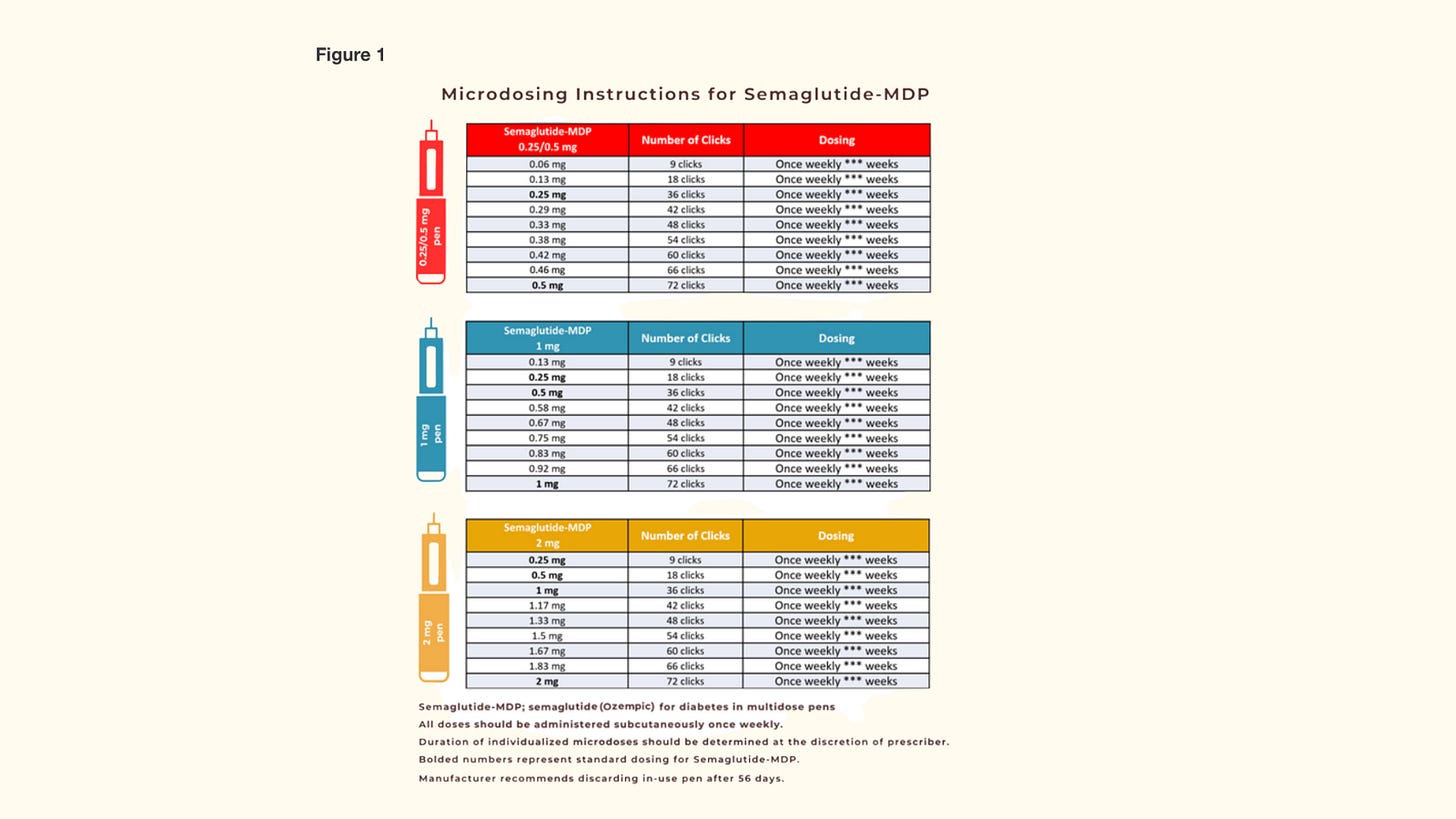
But as a method, fractional dosing feels archaic and clumsy.
What if patients miscount the clicks, or miss hearing them altogether? It's a messy compromise born purely out of necessity—and yet, despite these flaws, fractional dosing is spreading rapidly because clinicians and patients are desperate for flexibility.
This desperation is a signal that the market is practically screaming for a better, more precise dosing mechanism. Pens simply can’t deliver it, but vials can. Vials let you measure exactly the dose you need, offering true flexibility without counting clicks or relying on guesswork.
Vials aren’t mainstream yet, but the demand fractional dosing has created will inevitably push them there. If you're building in this space, keep a close eye on vials—they’re about to become your next big competitive advantage.
Conclusion
The truth is, if you can’t keep your patients, your business won’t survive. I don’t care how glossy your subway ads are, how bright your models’ smiles, how many millions you pour into branding—none of that matters if your patients spend their nights googling how to stop nausea or debating whether it’s worth spending another day constipated.
Your patients came to you because they were tired of feeling stuck. They came hoping to fit back into old clothes, to run around with their kids again, to finally feel in control of their health.
Predict side effects. Personalize doses. Keep your patients comfortable, engaged, and hopeful. Because the side effect you should fear most isn’t nausea or bloating—it’s watching your patients quietly disappear, right when they need you the most.
*The views, opinions, and recommendations expressed in this essay are solely my own and do not represent the views, policies, or positions of my employer or any other organization with which I am affiliated. This content is provided for informational purposes only and should not be considered medical or legal advice.*



I’m in the US, and I pushed through the side effects and didn’t go up in dose as long as I was losing weight (not diabetic). Never went higher than 5.0 Zepbound. Now, I’m at goal. I think the patient has to be determined to push through and stay the course. Aka, sometimes, you just have to suck it up!!!!
Blue Cross study done in US context with $1000 price tag. I am wondering if lower UK prices (thanks to NHS negotiated low prices) made a difference in retention. Any UK study?